Skilled Nursing Note - Matrix Home Care.
Skilled note. This is a medical record that documents a detailed and well-researched patient’s status. A skilled nursing note is detailed and includes the observation and suggestions of a healthcare provider about the condition of a patient. This note involves a lot of critical thinking and professionalism when writing. Nursing admission note.
A nursing note is a medical or health record that is made by a nurse that shows an accurate documentation of nursing assessments, changes in patient’s conditions, care provided, and related information to support the clinical team to deliver excellent care. First thing that goes on the nursing note is the patient’s information.

To write or not to write are equally important. Nursing documentation cannot be erased; once you write is there forever. If you make a mistake or forget something you can always write a late entry. But you can never delete a note from the records. So remember, the more important a situation is, the more you should think before you write. If in.
Hospice nursing visit is commonly done for those who are terminally ill. But that isn’t always the case, as scenarios would always differ from one another. The nurse on duty, referred to as a hospice nurse, still needs to take notes. There are also some hospice nursing visit note templates in Word. If you want to write one, you can.

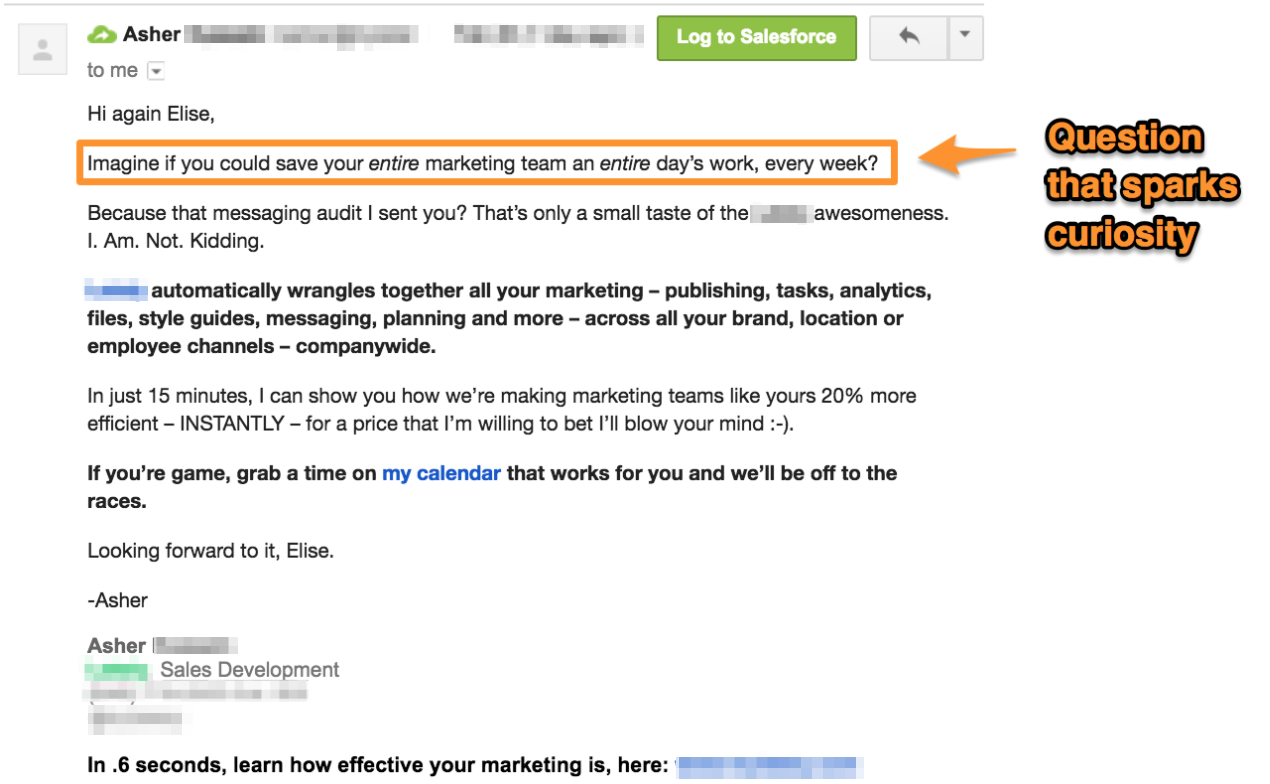
Tips for Writing Quality Nurse Notes Nothing matters more than providing clear and detailed information about a patient's condition and their symptoms on their chart. Your observations make it easier to determine what medical treatments a patient needs without serious mistakes being made.

The new skilled nurse note, scheduled for release January 2018, supports agencies with best practice processes, including clinical documentation improvement with embedded QA elements. The new skilled nurse note enhances the ease and quality of documentation, especially the patient’s need for skilled nursing services based upon their.

Nursing Service. pronursingservice.com. Helpful Tips When Writing a Nursing Note. A nursing note or documentation is a lasting collection of legal documents that should support an accurate report that focuses on the health condition of every patient. Nursing notes need to have sufficient data. This is to allow each nurse to provide utmost care.
Documentation Guidelines for Skilled Care. 2. Disclaimer The provider and instructor declare that neither has a conflict of interest in presenting this educational offering for the receiving entity. “What Makes Us Different, Makes You Better” 3. Objectives At completion of this program participants will be able to: Document to demonstrate implementation of the nursing process Document to.

What is a nursing note nurses write their nursing notes with to all their nursing notes Check out Practice Fusions free EHR system to. The Case For Nurses Notes - Providermagazine These resources will help you write on the job and in List of Nursing Resources provides links to Purdue OWL resources that both nurses and Note, even.

Note: this sample charting was from a patient with a recent CVA (Cerebral Vascular Accident or Stroke, a clot or bleed in the brain’s vascular system.) The areas of assessment you need to focus on depend on what is wrong with your particular patient.

Document a skilled nursing visit to a home care patient, as well as an aide supervisory visit when it is a part of a skilled nursing visit. Download a sample today!

From this lesson, you will learn why nurses use SOAP notes to write about patients, as well as what each section of the SOAP notes stand for along with specific examples.

Find this Pin and more on Nursing by Yeye Luke. sample nursing assessment form Example of narrative-chronological nurses' progress notes. sample nursing assessment form Example of narrative-chronological nurses' progress notes. Find this Pin and more on Sample Note Templates Documentation by Griffin Jude. Find this Pin and more on Quotes by.